In patients with acute coronary syndrome, decrease seen in cardiac death, MI, stent thrombosis with TiNO-coated stent, which was offset by increase in target lesion revascularization
By Elana Gotkine HealthDay Reporter
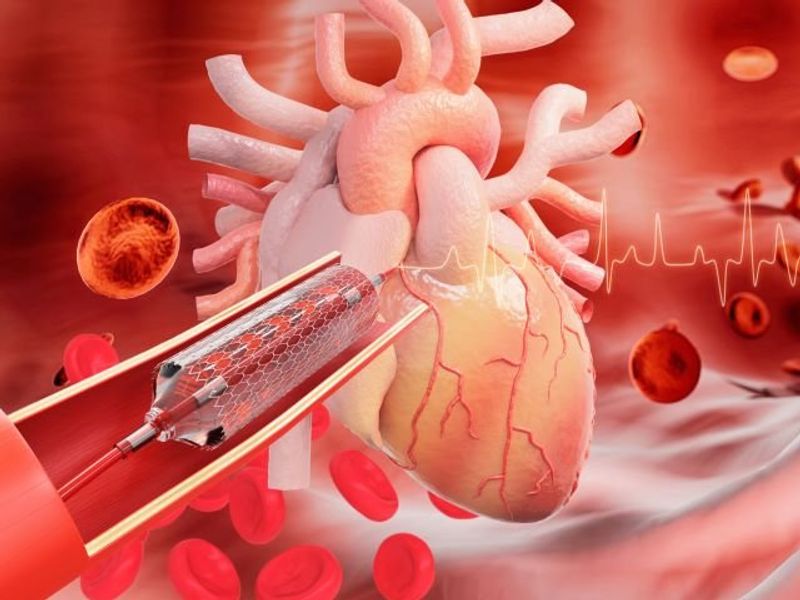
TUESDAY, May 30, 2023 (HealthDay News) — For patients with acute coronary syndrome (ACS), titanium-nitride-oxide (TiNO)-coated stents do not improve long-term outcomes in terms of a composite outcome over third-generation everolimus-eluting stents (EES), according to a study published online May 19 in JAMA Cardiology to coincide with EuroPCR, the official annual meeting of the European Association of Percutaneous Cardiovascular Interventions, held from May 14 to 17 in Paris.
Frederic Bouisset, M.D., from the Cardiovascular Center Aalst in Belgium, and colleagues compared the rate of the main composite outcome of cardiac death, myocardial infarction (MI), or ischemia-driven target lesion revascularization at five years in a multicenter randomized trial involving patients with ACS with at least one de novo lesion randomly assigned to receive either a TiNO-coated stent or a third-generation EES (989 and 502 patients, respectively).
The researchers found that the main composite outcome events occurred in 11.2 and 12.0 percent of patients in the TiNO and EES groups, respectively (hazard ratio, 0.94 [95 percent confidence interval, 0.69 to 1.28]; P = 0.69). In the TiNO and EES arms, respectively, the rate of cardiac death was 0.9 versus 3.0 percent (hazard ratio, 0.30 [0.13 to 0.69] P = 0.005); MI was 4.6 versus 7.0 percent (hazard ratio, 0.64 [0.41 to 0.99]; P = 0.049); stent thrombosis was 1.2 versus 2.8 percent (hazard ratio, 0.43 [0.20 to 0.93] P = 0.034); and target lesion revascularization was 7.4 versus 6.4 percent (hazard ratio, 1.16 [0.77 to 1.76]; P = 0.47).
“A significant reduction in cardiac death, MI, and stent thromboses in favor of TiNO-coated stents was offset by numerically higher rates of ischemia-driven target lesion revascularization,” the authors write.
Several authors disclosed ties to pharmaceutical and medical device companies, including Hexacath, which funded the study.
Copyright © 2023 HealthDay. All rights reserved.